Published: January 2015
Last Reviewed: March 2025
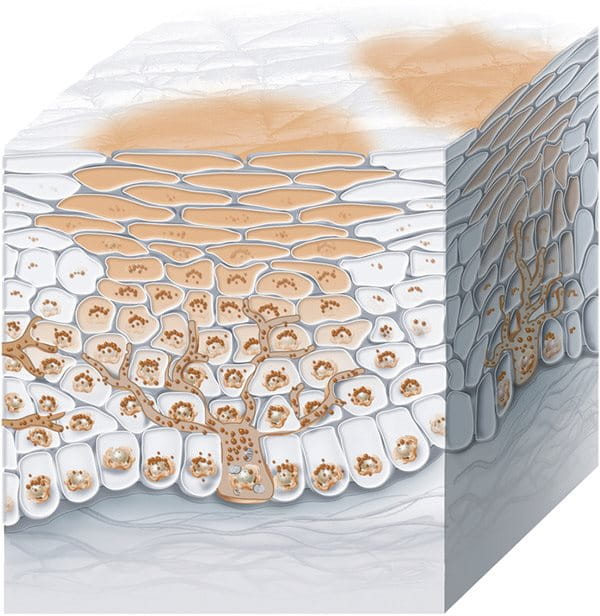
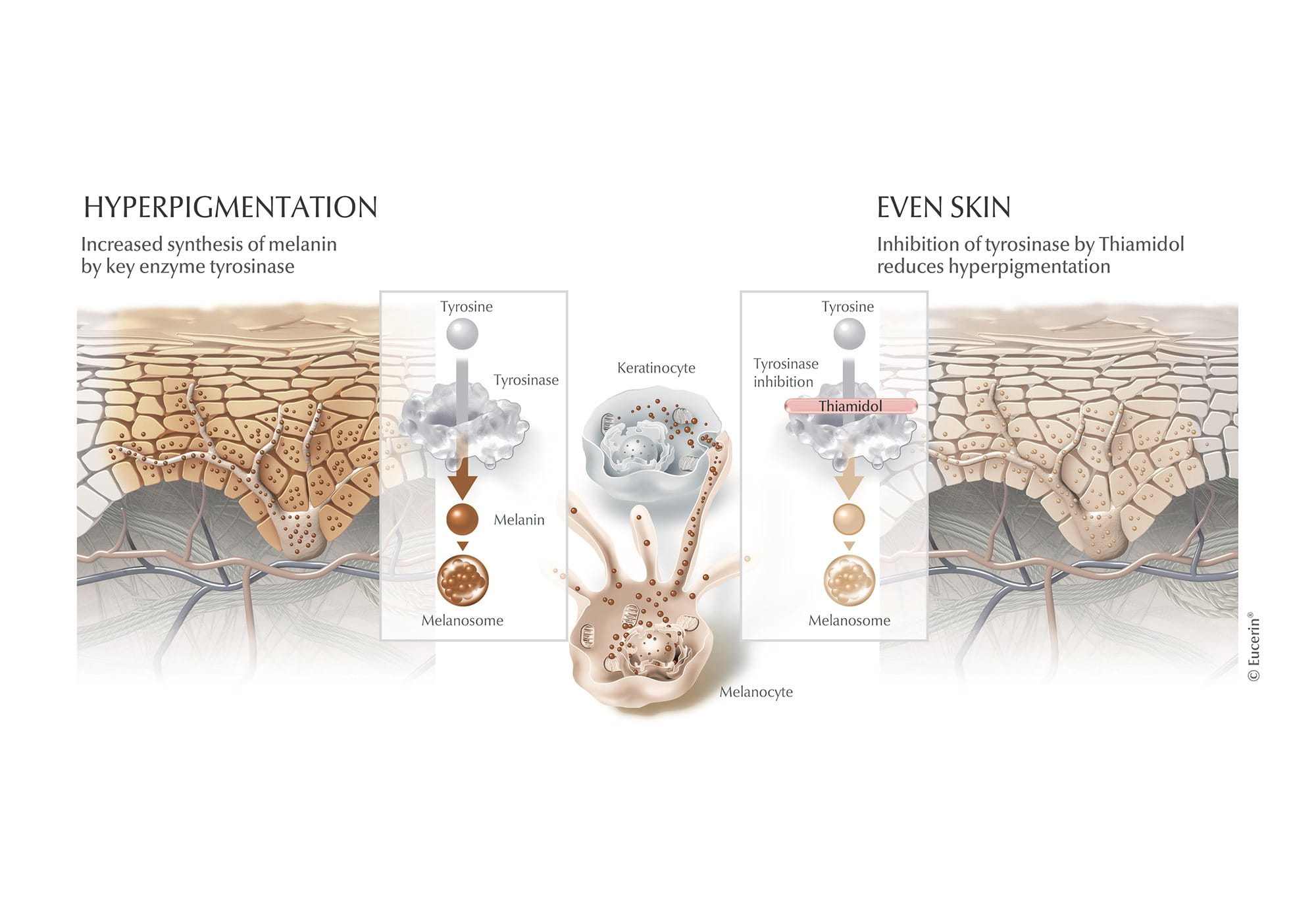
Melasma is a common skin condition that causes dark patches, usually on the face, leading to an uneven skin tone. It’s often called “the mask of pregnancy” or “chloasma” as it frequently appears during pregnancy due to hormonal changes. However, it can also be triggered by sun exposure, genetics, blue light, or birth control pills.
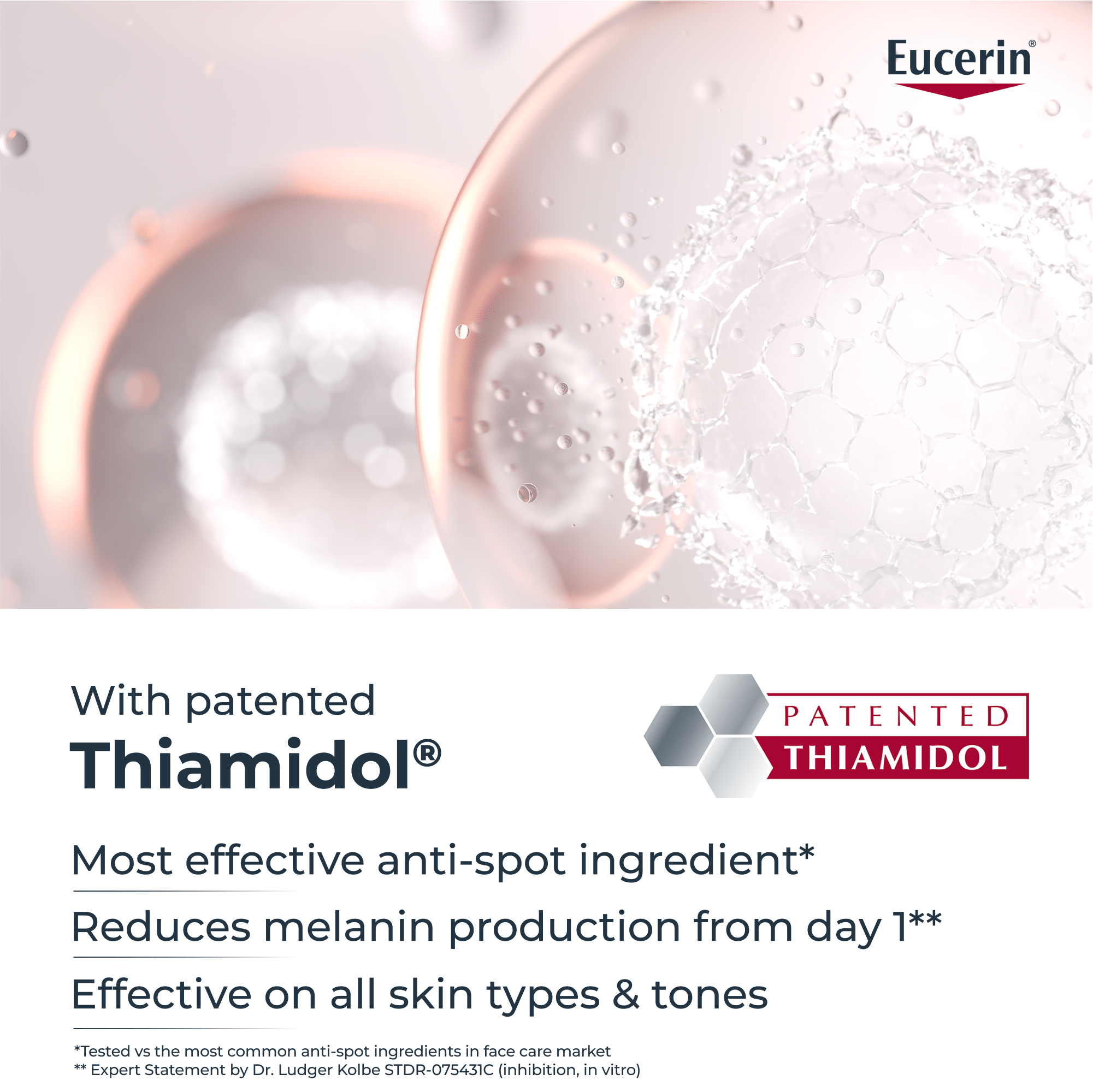
While melasma is harmless, it can be persistent. This article explores its causes, types, and effective treatments using dermatological skincare solutions. Learn how the Eucerin Anti-Pigment range can help reduce melasma and achieve a more even, radiant complexion.